Waymark
By: Waymark
Care, guided by community
We are trying to fill two key gaps in the Medicaid marketplace: (1) the need to synthesize a large amount of data from multiple disciplines (pharmacology, specialty care, psychiatry) to pick the right interventions for patients with multiple complex comorbid conditions and different preferences for treatment; and (2) the need to target interventions to the patients who would benefit most, and reduce polypharmacy among those patients who would face the most side-effects and least benefit, in the context of high demand and low supply of Medicaid providers. We provide a new workforce to serve Medicaid patients, and help that new workforce scale to address the growing population of patients insured through Medicaid (~100M people) through more efficient and more targeted interventions. We enable our care teams to focus on the highest-yield human interactions while using technology to help them know which patients to contact, when, and with what intervention. This reduces opportunity costs and helps our staff select interventions that maximize benefits and minimize risks to individual patients. Additionally, by making software that allows our staff to provide feedback on the algorithms, we fill the need to have direct provider feedback to machine learning algorithms. This feedback has been critical to identify biases in standard algorithms and address health disparities. For example, we found that the standard national algorithm for heart disease treatment systematically underestimated the risk of heart attacks for African-Americans, and were able to correct that bias [Ann Int Med, 2018, doi: 10.7326/M17-3011].
- Waymark is a public benefit corporation. Our mission is to enable community based care, using technology, to catalyze improvements in access and outcomes for patients receiving Medicaid benefits. We train community health workers, social workers, and pharmacists, and deploy them to primary care offices, patient homes, and community sites like food banks and homeless shelters--backed up by telemedicine resources including telepsychiatry and specialist e-consultation. We help patients with social barriers to good health (like getting housing, transportation, and food), mental health and substance abuse problems (through rapid and sustained mental health therapy), and challenges getting coverage for and adhering to their medications (by working with our advanced practice pharmacists to select and titrate chronic disease medications). We partner with health plans to deliver a set of interventions that are highly effective according to several randomized trials [Ann Intern Med, 2022, doi: 10.7326/M22-0074; Am J Manag Care, 2020, doi: 10.37765/ajmc.2020.42402; Health Aff, 2020, doi: 10.1377/hlthaff.2019.00981], but frequently unavailable to patients receiving Medicaid because of the lack of adequate workforce and technology to provide the interventions. Our key product is a set of technologies to make care more targeted and effective. We specifically develop machine learning algorithms delivered through our novel care management software to help our care team identify which patients to outreach at what time, match those patients to the right interventions, and improve the efficiency of our staff so they can address the high ratio of demand to supply of Medicaid care providers.
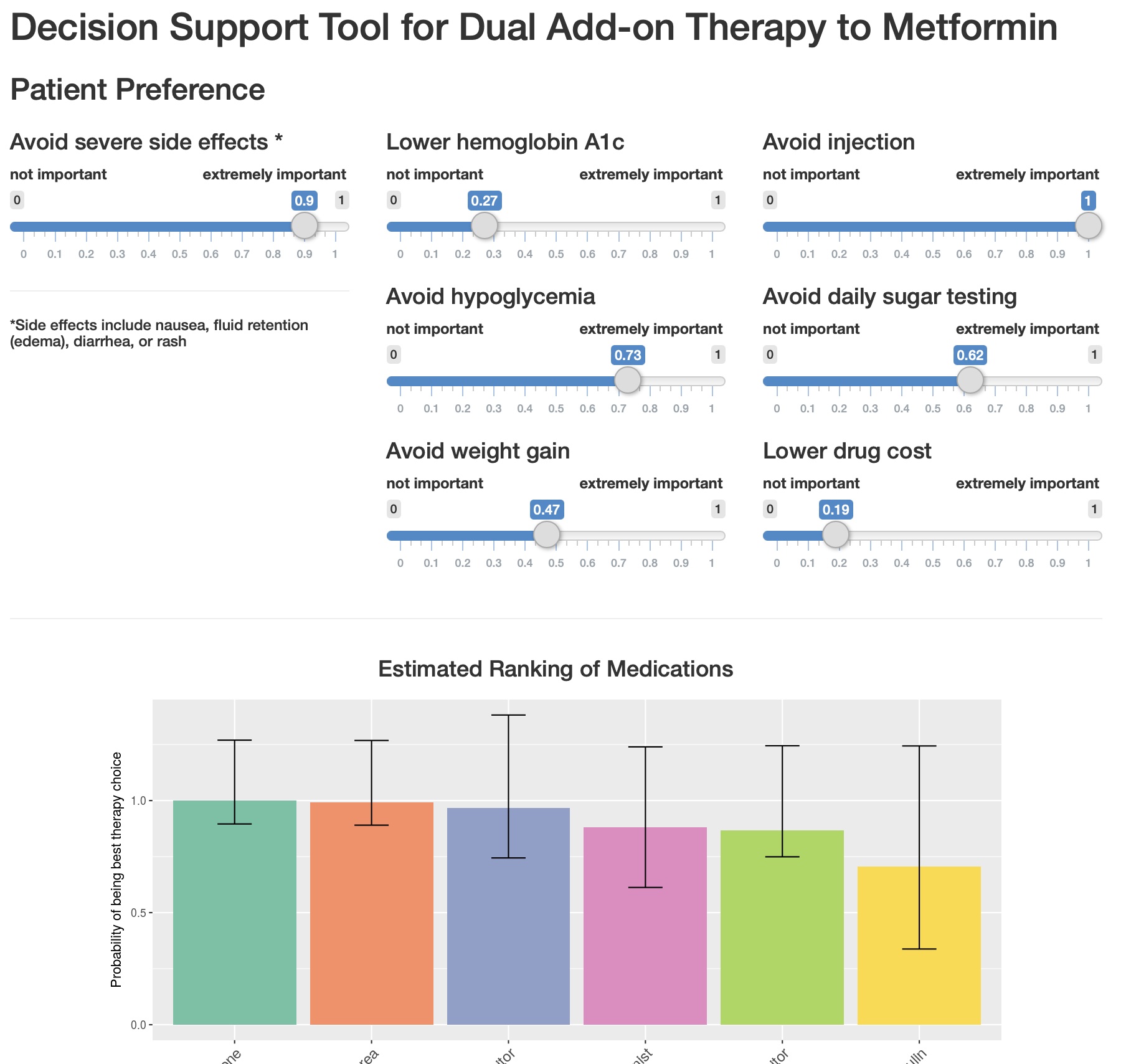
- Our differentiators include: (1) open-source algorithms to personalize the predictions of risks and benefits of alternative interventions for an individual patient; (2) open-source algorithms to help identify which patients to outreach and when; (3) peer-reviewed randomized controlled trial data underlying our data science and interventions; and (4) software that enables human feedback to continuously iterate on our machine learning technologies. We deviated from standard healthcare ‘risk prediction’ models that focus on predicting who will have a hospitalization or who will incur high costs. Instead, we developed and validated a set of machine learning algorithms that focus on which patients experience which benefits or which risks from a given intervention to lower their risks. For example, we trained our models to trials of intensive versus standard blood pressure treatment to identify which patients benefit versus experience harm from different blood pressure therapies [PLOS Med, 2017, doi: 10.1371/journal.pmed.1002410; Circ CQO, 2019, doi: 10.1161/CIRCOUTCOMES.118.005010]. We extended our modeling to diabetes [Diabetes Care, 2018, doi: 10.2337/dc17-2252; MDM, 2019, doi: 10.1177/0272989X19829735], diet/nutrition selection [BMJ Open, 2019, doi: 10.1136/bmjopen-2019-032703], depression treatment [JAMA Netw Open, 2020, doi: 10.1001/jamanetworkopen.2020.6653], and schizophrenia treatment choices [MDM, 2019, doi: 10.1177/0272989X19884927]. We applied our algorithms to network meta-analyses of RCTs to provide predictive comparisons across all available intervention choices and tailored them to patient preferences. Our software enables our care teams to rank our algorithm's results, providing feedback to improve our models.
- Released
- From a clinical ROI standpoint, our intensive blood pressure algorithm (N = 9,069 for derivation, N = 4,498 for validation) for our pharmacist-provider dyads would be expected to avert 900,000 more cardiovascular disease events, saving 2.8 million more quality-adjusted life-years (QALYs) if scaled nationwide than using the standard national guideline [Circ, 2013, doi: 10.1161/CIRCULATIONAHA.113.002290]. Our algorithm for schizophrenia therapy selection (N = 13,054) to help therapist-psychiatrist dyads choose the right treatments improved patient’s quality of life by 0.33 QALYs per patient, versus the standard guideline [MDM, 2019; doi: 10.1177/0272989X19884927]. Similarly, our diabetes algorithm (N = 595,700) would be expected to avert 14 cases of emergency department visits or hospitalizations unaddressed by standard care per 100,000 people with diabetes [Med Care, 2017; doi: 10.1097/MLR.0000000000000728]. From an economic ROI standpoint, the overall care team interventions have a return of investment of $2.47 in reduced healthcare costs per $1 invested in the program [Health Aff, 2020, doi: 10.1377/hlthaff.2019.00981]. Our hypertension algorithm was incrementally cost-saving, at $1,187 per QALY [BMJ Open, 2017, doi: 10.1136/bmjopen-2017-018374], with disproportionate benefit to minorities (reducing Black-White disparities from 23.1 to 3.6 excess events per 1,000 Black adults) [MDM, 2017, doi: 10.1177/2381468317725741]. Our diabetes algorithm has an incremental savings of $2900 per QALY saved [MDM, 2019, doi: 10.1177/0272989X19829735]. And our food insecurity algorithm would be expected to avert $54.1 million per year in emergency department and inpatient hospitalization costs if scaled nationally [Med Care, 2017; doi: 10.1097/MLR.0000000000000728].
- N/A
- --
 My Rx Pad
My Rx Pad 


 Product Link
Product Link.png)